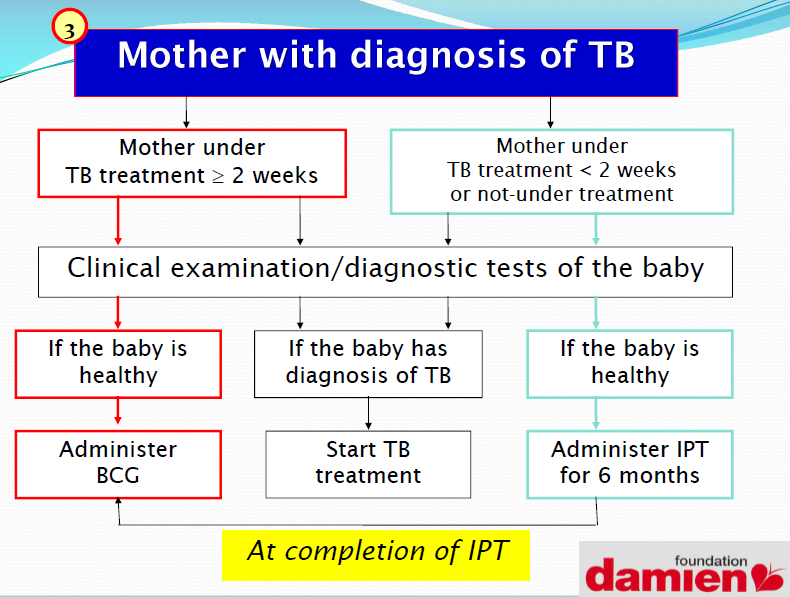
Young children living in close contact with a source case of smear-positive pulmonary TB are at particular risk of TB infection and disease.
The risk of infection is greatest if the contact is close and prolonged such as the contact an infant or toddler has with a mother or other caregivers in the household.
The risk of developing disease after infection is much greater for infants and young children, especially those under 3 years.
How Children are infected?
- From coughing adult
- From infected milk (bovine TB)
- Through the skin
- From pregnant mother if she is not on treatment

Congnital TB
Congenital TB can result from:
- Heamatogenous dissemination of M. t after maternal mycobacteremia,
- Rupture of a placental tubercle into the fetal circulation,
- Ingestion of infected amniotic fluid or maternal blood at delivery. The mother might not have symptoms of TB disease,
and subclinical maternal genital TB also can result in an infected neonate
Diagnosis of TB in Children
- Careful history (including the history of TB contact & symptoms consistent with TB)
- Clinical examination (including growth assessment)
- Tuberculin skin testing
- Bacteriological confirmation whenever possible
- Investigations relevant for suspected pulmonary TB and suspected extrapulmonary TB
- HIV testing (in high HIV prevalence areas).
Suspecting TB in Children
- Low-grade fever not responding to malaria treatment
- Night sweats
- Loss of weight
- Loss of appetite
- Failure to thrive
- Lymph node swellings
- Joint or bone swellings
- Angle deformity of the spine
- Listlessness
- Neck stiffness, headache, vomiting (TB meningitis)
Risk Factor in TB
- Household contact with a newly diagnosed smear-positive case
- Age < 5 years
- HIV infection
- severe malnutrition.
Main Feature Suggestive of TB.
The presence of three or more of the following should strongly suggest a diagnosis of TB:
- Chronic symptoms suggestive of TB
- Physical signs highly of suggestive of TB
- Appositive tuberculin skin test
- Chest X-ray suggestive of TB.
Systoms
The commonest are:
- Chronic cough
– An unremitting cough that is not improving and has been present for more than 15 days. - Fever
– Body temperature of >38 °C for 14 days, after common causes such as malaria or pneumonia have been excluded. - Weight loss or failure to thrive
– In addition to asking about weight loss or failure to thrive, it is necessary to look at the child’s growthchart.
Important Physical Signs are:
. Physical signs highly suggestive of
extrapulmonary TB:
- Gibbus, especially of recent onset (resulting from vertebral TB).
- Non-painful enlarged cervical lymphadenopathy with fistula formation.
Physical Signs Requiring Investigation to Exclude Extrapulmonary
- Meningitis not responding to antibiotic
treatment. - Pleural effusion.
- Pericardial effusion.
- Distended abdomen with ascites.
- Non-painful enlarged lymph nodes without fistula formation
- Non-painful enlarged joint.
Documented weight loss or failure to gain weight, especially after being treated in a nutritional rehabilitation programme, is a good indicator of chronic disease in children, of which TB may be the cause.
Tuberculosis Skin Test.
- The TST should be standardized for each country using either 5 tuberculin units (TU) of tuberculin purified protein derivative (PPD)-S or 2 TU of tuberculin PPD RT23, as these give similar reactions in TB-infected children.
- A TST should be regarded as positive as follows:
- in high-risk children (includes HIV-infected children and severely malnourished children, i.e. those with clinical evidence of marasmus or kwashiorkor): >5 mm diameter of induration;
- in all other children (whether they have received a bacille Calmette–Guérin (BCG) vaccination or not):
Bacteriological confirmation whenever possible.
Appropriate specimens from the suspected sites of involvement should be obtained for microscopy and, where facilities and resources are available, for culture (and also histopathological examination).
Appropriate clinical samples include:
- sputum,
- gastric aspirates and certain other material (e.g. lymph node biopsy or any other material that is biopsied).
- Fine-needle aspiration of enlarged lymph glands – for both staining of acid-fast bacilli and histology – has been shown to be a useful investigation, with a high bacteriological yield.
Gastric Aspiration
B) If still < 5 – 10 cc of gastric contents have been aspirated, put any yield into your cup or tube.
CC: Damien Foundation.
Thank you for reading, kindly bear your mind out on the comment section or ask your question(s) in the comment box on the topic: Tuberculosis (TB) in Children. Kindly share this post link with your friends and on your social media handles.

Pingback: Diabetes and Its Prevention | AMOHN Lagos State
Pingback: Tuberculosis, Prevention, Symptom and Cure - AMOHN LC
Pingback: Vaccines and Immunization - AMOHN LC